This article explains whether dental implants may be possible for people with osteoporosis, what a thorough diagnostic workup should include, and how modern techniques and aftercare can improve safety and outcomes—so even older patients can make decisions with more confidence.
“I have osteoporosis—can I still get a dental implant?”
“I’m older and my bones are weak. What if surgery makes things worse?”
Have you ever lost sleep over these questions?

These are among the most common questions osteoporosis patients ask in the dental chair.
For many older adults, the fear is not only about missing teeth, but about a deeper concern: “Is it safe for me to undergo surgery at all?”
Online, you may also see exaggerated claims like “If your bones are weak, implants are absolutely impossible,” which can increase anxiety.
Don’t worry—this is not meant to scare you. Based on the types of cases clinicians see every day, this guide will walk you through how to assess whether implants may be an option for osteoporosis patients, step by step.
We’ll focus on the question “Can implants be possible with osteoporosis?”—why it was once considered difficult, what diagnostic tools and solutions exist today, and what you should confirm before treatment.
The goal is to replace uncertainty with clear, practical information.
1.Why can implants be more challenging in osteoporosis?
In the past, implant success rates in osteoporosis patients were thought to be lower. When bone density is reduced, initial stability can be weaker, and the bone-to-implant bonding process (osseointegration) may be delayed or more likely to fail.
In addition, long-term use of osteoporosis medications (such as bisphosphonates) has been associated with a risk of jawbone osteonecrosis, leading some patients to avoid implant treatment altogether. However, this perspective was largely shaped by limited clinical data from the 1990s to the early 2000s.
Modern implant dentistry has advanced significantly. Rather than concluding “You can’t,” the right approach today is often: “How can we make it possible—safely?”
| Healthy Jawbone | Jawbone with Osteoporosis | |
|---|---|---|
| Bone condition | Higher bone density with a tight, well-organized internal structure. | Lower bone density with a more porous, “spongy” internal structure, which can be weaker. |
| Implant stability (initial fixation) | The implant typically achieves strong initial stability because it anchors firmly in the bone. | Achieving strong initial stability may be more challenging, as the implant may not anchor as firmly at first. |
| Osseointegration | Bone cells tend to attach and remodel actively around the implant surface, supporting more predictable integration. | Bone remodeling capacity may be reduced, so osseointegration can take longer and may be less predictable in some cases. |
| Key message | Beyond what you see on imaging, the bone’s internal quality and biological environment can strongly influence implant outcomes. | Bone quality can affect early stability and healing—so individualized assessment and planning are especially important. |
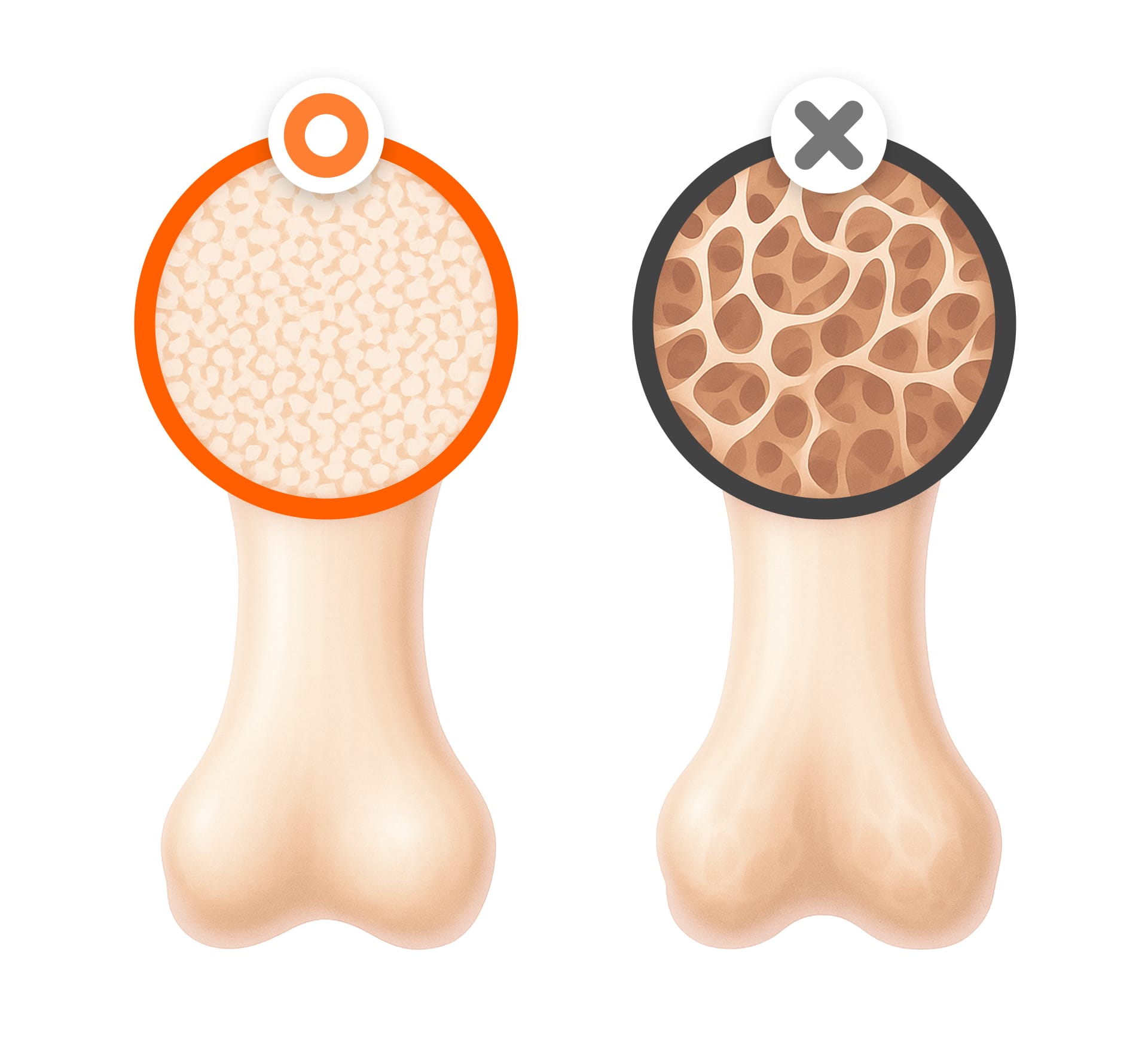
2.The key to implant success: bone volume vs. bone quality
You may have heard, “I don’t have enough bone, so I can’t get an implant.” But implant outcomes are not determined by bone volume alone. In practice, bone quality plays a particularly important role in early stability and healing.
Bone quality refers to the internal strength and biological environment that helps an implant anchor securely and heal predictably.
Our bones have two main structural components: cortical bone (a dense outer layer, like tree bark) and trabecular bone (a spongy inner network with rich blood supply). Early on, implants rely heavily on cortical bone for stability. Over time, long-term stability depends on healthy osseointegration supported by the trabecular structure.
- Cortical bone: Dense outer layer; critical for initial stability
- Trabecular bone: Spongy inner structure; supports long-term osseointegration
In osteoporosis, trabecular bone density may be reduced and can affect implant stability. However, if CT imaging confirms strong cortical bone in a suitable area, stable outcomes may still be achievable.
Today, clinicians increasingly evaluate bone quality using a multi-factor approach—not only numbers, but also age, hormonal status, and nutritional status.
For example, even a woman in her 70s may achieve excellent initial stability in certain areas if cortical bone quality is favorable.
[How bone volume and quality influence implant outcomes visual]
| Factor | Bone Volume (Quantity) | Bone Quality |
|---|---|---|
| How it’s assessed | Bone thickness and overall volume | Bone density, healing capacity, and internal structure |
| Impact on implants | Supportive (helps planning and long-term support) | Often critical (strongly influences early stability and healing) |
| Primary role | Long-term support and stability | Initial fixation and osseointegration |
3.Why “accurate diagnosis” is essential for osteoporosis patients

A safe implant plan begins with a thorough diagnostic workup. This goes beyond standard dental X-rays and should include overall health status and medication history.
- 3D CT scan: Assesses bone thickness, density, and nerve location in three dimensions, enabling precise implant length and angle planning.
- DEXA scan: Evaluates overall bone mineral density. Comparing spine/femur values with jawbone findings can help estimate surgical safety.
- Medication history: Whether you use bisphosphonates or denosumab, for how long, and at what dose—these details matter and can change the plan.
- Blood tests: Helps review inflammation markers, immune status, and bleeding risk to reduce postoperative complications.
- Lifestyle assessment: Smoking, alcohol use, and oral hygiene habits can directly affect healing speed and stability.
4.Modern implant solutions—even when bone is weaker

Modern dentistry offers multiple strategies to address limitations commonly seen in osteoporosis patients:
- Special surface-treated implants: Designed to promote faster bone cell attachment and potentially improve osseointegration speed.
- Digital guided surgery: CT-based simulation helps place implants at the safest angle and position, reducing complications.
- Short implants and angled placement techniques: Can help secure stability even in areas with limited bone volume.
- Advanced bone graft materials: Synthetic grafts, autografts, and allografts can reinforce deficient bone. Some clinicians may also use growth-related approaches (e.g., PRF, BMP) to support regeneration.
5.The final key to success: osseointegration
Ultimately, implant success depends on whether osseointegration—the bond between the implant and bone—develops well. In osteoporosis, bone regeneration can be slower, and failure risk may exist.
To support osseointegration, clinicians may combine surface-treated implants, strategies to secure strong initial stability, careful lifestyle management, and regular follow-ups. For example, studies have reported that smoking can more than double the risk of osseointegration failure—so smoking cessation is strongly encouraged.
During recovery, calcium and vitamin D supplementation and balanced nutrition can support healing. For at least 3–6 months, it is important to avoid excessive chewing forces and to monitor implant stability through periodic clinical and imaging evaluation.
6.Frequently asked questions(FAQ)
Q. I have osteoporosis—can I still get implants?
Osteoporosis does not automatically mean implants are impossible. If CT imaging confirms a stable bone structure and an appropriate site is selected, success rates may be similar to those in patients without osteoporosis. However, healing may take longer, so careful follow-up is important.
Q. Should I stop my osteoporosis medication before surgery?
Do not stop medication on your own. Stopping may worsen overall bone health. Because bisphosphonates and denosumab have been associated with jawbone osteonecrosis, planning should be coordinated with your prescribing physician and dental clinician. Dose timing or scheduling may be adjusted based on individual risk.
Q. My bone volume is limited—can implants be done without bone grafting?
In some cases, short implants, angled placement, and digital guided surgery may reduce the need for grafting. However, this is not suitable for everyone—bone quality and systemic health must be considered. A thorough evaluation is the safest way to choose the best approach.
Q. What is the most important lifestyle care after surgery?
The first 3–6 months are the critical osseointegration phase. Avoid hard foods, maintain excellent oral hygiene, and keep scheduled follow-ups. Calcium/vitamin D support and habits such as no smoking and limiting alcohol can meaningfully improve long-term stability.

Many people feel anxious about getting dental implants when they have osteoporosis. However, with a thorough evaluation and an individualized treatment plan, it may be possible to achieve stable and predictable outcomes. The key is a personalized approach—one that considers bone condition, medication history, and lifestyle factors together. Rather than relying on fear or assumptions, aim to reduce uncertainty with accurate information and professional guidance so you can make the healthiest decision for your situation.
Sources
- Pjetursson, B. E., et al. (2014). Implant survival in patients with osteoporosis. Clinical Oral Implants Research, 25(7), 819–826.
- Roca-Millan, E., et al. (2021). Osteoporosis and dental implants: A systematic review. Journal of Clinical Medicine, 10(5), 1032.
- Korean Academy of Oral & Maxillofacial Implantology. (2022). Clinical guidelines for implant treatment in elderly patients.
※ The copyright for all content on this blog belongs to Medihigh. Unauthorized copying, distribution, or derivative use is strictly prohibited, and violations may result in legal action without prior notice.
Recommended reads